Have you ever had your Doctor/Physiotherapist/Chiropractor tell you “your joint is all bone on bone”, “your spine is full of arthritis”, or “you blew out your disc”? Have you ever had a friend describe their condition like “I have the back of a 70 year old” or “I have a bad _____ (insert back/knee/hip)”? Healthcare professionals have many important responsibilities, including assessing a patient, screening for serious pathology, and delivering a proper diagnosis. What is even more important, is educating a patient on their condition and it is a responsibility that requires a certain skill. There is an art to presenting enough information to the patient so they understand the nature of their pain while framing it in a non- threatening way. The terms and the language we use to explain our findings and diagnoses influence the way that our patients respond to our treatment.
This may be a bold statement, but the way we present information to our patients is crucial. Using our words we can either set our patients on a path to a successful recovery or doom them to avoid movement due to fear of producing further damage. This is best illustrated by looking at the fear avoidance model of pain, first proposed by Lethem et al. in 1983. Following an injury, if the patient interprets their pain as very threatening they will begin to catastrophize their pain.

When an injury occurs and a person receives very threatening information about their diagnoses they begin to catastrophize their pain. Catastrophizing means focusing on negative thoughts, such as believing they will never be able to be rid of their pain, that things are only going to get worse, and feeling helpless about their situation. Another damaging idea is pain must be avoided at all costs and bed rest is the best solution. This leads to inactivity and disuse, the consequences of which are ultimately muscle atrophy, dysfunction, depression, and more pain.
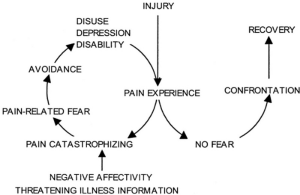
The path a patient will follow is largely dependent on factors such as their personal coping mechanisms, previous experiences, level of previous activity etc. However, health professionals have a large role to play in directing a patient towards the right path – leaving them confident that change is possible or helpless about their fate. For example, a patient who has suffered from knee pain for a very long time is told that their knee is “worn out” their joint is “bone on bone” and they probably should be very careful from now on. This patient is going to be a lot less likely to keep moving, they will be hyper-vigilant about their pain, and will be less motivated to initiate an exercise program. Of course inactivity actually snowballs the problem, leading to more stiffness, dysfunction, and ultimately more pain.
Breaking the negative thought cycle is extremely difficult and the best approach is to set somebody up for success right from the start. Making patients feel like they are broken with ominous statements about their health does a lot more harm than good.
Below I have outlined my three least favorite statements as repeated by patients about their back pain:
“Degenerative disc disease”
This may be my least favorite statement to see on a patient’s x-ray results. Hearing you have “degenerative disc disease” is extremely frightening as it sounds like a progressive, threatening disease where pain will only get worse. This typically conjures up images of hunched backs, wheelchairs, and severe disability. Degenerative disc disease is a misnomer and refers to the approximation of the vertebrae of the spine, which is a part of the normal aging process. Anybody over the age of 20 will start showing some radiographic changes in their spine. Labeling it as a “disease” gives the impression that the patient is one of a small number of people afflicted by this condition.
So if it happens to all of us why do some of us have pain and others don’t?
This is how it typically goes: patient has back pain —> they are sent for an x-ray/MRI —> the imaging shows degenerative changes (I would be very surprised if it didn’t) —> patient is diagnosed with degenerative disc disease. However, the pain they experience has nothing to do with these changes and everything to do with they way they move- using dysfunctional movement patterns and placing their spine under excess load. Giving somebody the diagnoses of “degenerative disc disease” makes them think that they should guard their “fragile” spine as much as possible – resulting in way bigger dysfunction
“Threw out your back”
What a colorful way to describe symptoms of a sudden severe back pain and stiffness. “Threw out your back” makes it sound as if significant, irreparable damage has been done to the back, almost as if the joints of the spine literally shifted out of place and locked up. This type of pain comes on suddenly while performing a physical activity. It occurs in people who tend to move from their back instead of their hips and have poor core activation. Both of these factors create excess load through the spine on a daily basis, typically with no real symptoms. However, when the same person decides to move suddenly, creating even more load through the spine, the body goes into protective mode. The muscles around the area seize up, attempting to protect the body from the perceived harm

A back injury can be quite alarming and allowing somebody to keep referring to their injury as “throwing out the back” creates an unnecessary sense of doom. How likely would a patient be to adhere to an exercise program when they are scared that they are going to throw out their back again? This sort of thinking yields to other statements such as “I have a bad back” and “I have the back of a 80 year old”. Your back is fine. You are just asking it to do more than it was intended to.
“Bone on Bone”
“Bone on bone” is a common way to describe severe osteoarthritis. In osteoarthritis, cartilage, the slippery material that coats the end of bones, wears out producing symptoms of stiffness, pain, and swelling. Osteoarthritis effects weight baring joints such as the knee, hip, and spine. A patient who is suffering from knee, hip, and spine pain needs to be educated on what to do in order to place less load onto their joints- through movement, weight loss, bracing etc. The last thing they need to hear is that their joint is “bone-on-bone”. What a horrible, scary, unpleasant image to put into somebody’s mind- their bones literally grinding on one another. Again, how likely is this person to participate in activities and take on an exercise program?
One of the hardest jobs of a physiotherapist is convincing our patients that they are not broken! They can lead very active and healthy lifestyles, if only they stop the negative thinking and the guarded behavior. Breaking this negative cycle can be hard, especially after years of chronic pain- but it is possible and a good physiotherapist can help!
Yulia